Some years ago, after a bout of plantar fasciitis etc (yes, unpleasant), I went for a series of myofascial release treatments.
Now, I had countless massages over the years, and previous myofascial sessions with the therapist, but none of them elicited the response this particular movement up the leg did – it was I think somewhere on the adductors, but I cannot swear to this.
All of a sudden I was back to the age of 21 or so and fighting off a very powerful drunken male who was well known to me, who had simply carried me into his tent on an impulse and was attempting to assault me. Fortunately I am also very strong and had legs of iron. All I mostly remember is that he commented how strong my legs were. And until that moment on the couch, I had not thought about the incident for probably 30 years.
But my body had carefully stored the trigger, ready for the right touch to elicit the memory.
The figure of 97% of women having experienced sexual harassment and worse has recently been ringing loud in our ears and Tim Kiely, criminal barrister, has commented that there is a “social, political and cultural environment that is, knowingly and unknowingly, hostile to women …. which treats violent male behaviour towards women as a set of given, taken-for-granted circumstances which it is somehow the job of women to navigate”. https://www.openaccessgovernment.org/violent-male-behaviour/106138/
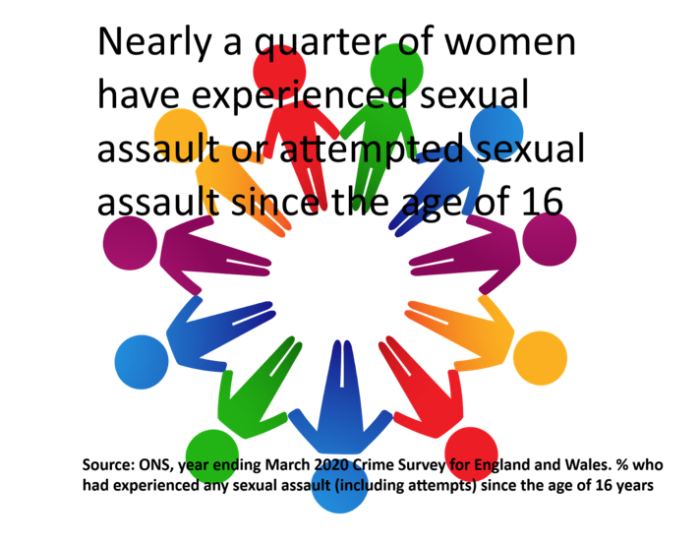
Although the ‘true’ figures for sexual assault may never be known, there are so many women (and men) who have stories they rarely share, and even less rarely report. It is, perhaps, odd, that given this almost commonplace incidence that there seems to be very little overt discussion in hands-on therapies of the implications for client handling in bodywork. There might be some discussions around client body language and what it might be suggesting. In your own practices, whilst clients may not disclose it is likely there are times when you may have noticed muscle guarding or particular changes in breathing, facial expression, flinching, shaking or similar?
Not all clients may share immediately a flashback with a therapist. They may feel the need to be given ‘permission’ to speak during treatments’. But how would you handle it, if they did? Or how have you handled it in the past?
One of the reasons I felt the need to write this article is that I did share the flashback (not in detail, but in general). The therapist I was working with at the time responded with something like ‘Oh ok’ and that was all. From the point of view of the person on the couch this really did not meet my needs.
I think what I would have been happy with was validation, acknowledgement and perhaps a gentle question as to whether it would help to talk with someone about this along with a relevant referral to a local professional. In addition, the question as to whether I wanted to end the session at this point might have been best practice.
What it did not require, however, was to turn a physical therapy session into a counselling session, particularly without appropriate skillsets.
I also think that this incident suggests that huge investments in technical skill sets, particularly ones that focus on the fascia, which from experience seems to be a real repository of emotion, needs also to be accompanied by training in communication skills and what I would call ‘holding the space’ skills together with a repertory of professionals to call upon. The therapist was very skilled and knowledgeable in this area, but was let down by training which had perhaps failed to prepare her how to handle these kinds of situations.

In researching for this article, I came across an interesting case study from 2012, published in the Physical Therapy and Rehabilitation Journal that you may like to read:
Kim Dunleavy, Amy Kubo Slowik, Emergence of Delayed Posttraumatic Stress Disorder Symptoms Related to Sexual Trauma: Patient-Centered and Trauma-Cognizant Management by Physical Therapists, Physical Therapy, Volume 92, Issue 2, 1 February 2012, Pages 339–351, https://doi.org/10.2522/ptj.20100344
This concludes with the statement “Physical therapists will be more effective if they are informed about psychological issues that influence their patient interactions and treatment. Although PTSD symptoms can present unexpectedly and pose challenges for the patient and physical therapist to manage, patient-centered management may assist with developing sufficient trust for disclosure. Further refinement of interactions and choices to provide trauma-cognizant care may assist patients with PTSD or a history of sexual trauma in controlling symptoms while addressing rehabilitation needs.”
It is well worth a read as there is much helpful and interesting content.
Rosemary Pharo
ThinkTree Hub Managing Consultant